“One fewer plate at the table” – the Grace Schara wrongful death trial.
With transcripts on informed consent and a biodefence ending.
ExcessDeathsAU is not on social media: I rely on you to share articles.
Please note: subscription billing is paused and I am currently demonetising my work. Read why here. Articles have always been free and will remain so.
Disclaimer: Not legal or medical advice. Reader discretion advised.
Dear Readers,
This was the most complex and harrowing article I have ever written. Even after everything that has occurred in the past five years, there were many times that I could not believe what I was hearing while listening to this trial.
At some points it was like the floor had dropped out from under me.
The first and most important message of the article is this: one must listen to the entire trial to form one’s own understanding of what occurred in that courtroom. I have manually typed transcripts and I encourage people to take the time to read them to increase understanding and how they relate to the ‘bigger picture.’ However, again, there is no substitute for listening to the entire trial.
Much of what happened these past five years are beyond my, or perhaps, if the reader will permit me, human understanding. I wrestled deeply with what I heard in that small courtroom in Wisconsin.
The case of Grace Schara was historic because (among other events) we finally had the chance to hear from the people who worked in the hospitals during covid Emergency powers in a courtroom under oath.
I previously reported on Grace’s case including covid hospital protocols during Emergency powers over multiple articles which may be found linked here:
Grace Schara was a 19-year-old woman from Appleton, Wisconsin who lived with Down Syndrome. She was never vaccinated for covid. Grace was admitted to Ascension St. Elizabeth Hospital after presenting to a local Emergency department with ‘covid symptoms.’ The family did not want Grace to be intubated. While Grace was in the hospital, “do not resuscitate” (DNR) and “do not intubate” (DNI) orders were placed in her records by physician Dr Gavin Shokar. Grace’s mother, father, and sister Jessica were recorded as powers of attorney (POAs) with Grace’s father Scott as the ‘main decision maker.’
During her hospitalisation for ‘covid symptoms,’ Grace was administered opiates and sedatives. She was never prescribed Remdesivir, Midazolam, or any emergency use authorisation (EUA) drugs specifically for ‘covid symptoms.’
On October 13, 2021, Grace died in the ICU. Despite the screams of Grace’s family to save her (Jessica in person and Mr and Mrs Schara via phone), no effort was made by the medical staff to revive her that did not involve intubation due to the DNI/DNR orders.
The trial examined allegations of negligence, lack of informed consent, and medical battery. The plaintiff1 also [sought] a declaratory judgment for the DNR order and medication combination that the plaintiff alleges resulted in his daughter’s death.
Note that the medical battery was thrown out by the judge during the trial.
At the end of the trial, the jury ruled in favour of the defence (Ascension Hospital et al.) after a short (ca. 15 minute) deliberation. (Archive).
Again, Grace was never prescribed Remdesivir or Midazolam as we saw in so many other cases around the world during Emergency powers. She was never prescribed any emergency use authorisation (EUA) medications. The trial focussed mainly on the drugs Precedex and Lorazepam which, according to the medical experts who testified (doctors, nurses, toxicologist, pharmacist), are routinely used in intensive care units even outside covid emergency powers.
Evidence presented in this trial was largely concerned with the effect of Precedex and Lorazepam in an ICU setting and informed consent regarding DNRs. Key implications not explicitly investigated in the case are about what happened during covid times not just in the US but the rest of the world.
#
On the second day of the trial, Mr Schara, Grace’s dad, said there were four main reasons for filing the lawsuit: [Ed. - changed a few words in points 2 and 3 July 16, 2025 to reflect official court transcript provided here].2
Repentance of the individuals involved – that they may turn away from their sin.
Stop the behaviour.
Shed light on evil.
Change Grace’s death certificate to reflect the truth.
Therefore, the purposes of this article are to: 1) honour Grace Schara’s legacy and the advocacy of her family, 2) provide key points and lessons that emerged from the trial, and 3) supply transcript excerpts for reader understanding and the historical record.
With thanks to the Schara family, Children’s Health Defense (CHD.TV), NewAmerican, Wisconsin Circuit Court Access, and Grace.
Yours Faithfully,
ExcessDeathsAU
20 You intended to harm me, but God intended it for good to accomplish what is now being done, the saving of many lives.
Genesis 50:20. NIV. Full chapter.
Article outline
Essential links
Preamble
Transcripts: Informed consent in an intensive care unit.
Bonus mini-transcript: Nurse Alison Barkholtz makes a slur in court and nobody objects.
Final thoughts
#
Postscript: Building the future of biodefence at the speed of relevance with Dr David Fisk, MD., expert witness for the Defence.
1. Essential Links
Watch the full trial plus family press conference (courtesy of Children’s Health Defense).
Wisconsin Circuit Court Access: Outagamie County Case Number 2023CV000345 Scott Schara et al vs. Ascension Health et al.
Daily coverage of the trial (Archive) by Rebecca Terrell of New American (I have only skimmed this, has a particular viewpoint. Includes YouTube videos).
Schara family website ‘Our Amazing Grace.’
Photos of Grace and family in local news: “See Grace Schara, woman at center of wrongful death trial, billboard campaign.”
2. Preamble
In order to write this article I listened to the entire trial: nearly 104 hours3 over many weeks. With respect and thanks to those who made the trial available to me in Perth, Western Australia, much of the audio was poor which made this task extremely challenging.
In my quest for understanding, I listened to every single person who took the stand unfiltered as well as all the attorneys. I listened to what the judge allowed and how he interacted with every person in the courtroom. I listened to the machinations of evidence labelling and admission and all the legal discussions while the jury was on breaks. I listened to issues with how the court was organised and any issues that may have arisen with the physical location of the trial and the building itself.
I also listened carefully to the questions the jury asked to get a sense of what they wanted to know and how they may have arrived at their verdict.
Essentially, I tried to understand what was happening in the trial while also having the knowledge of Operation Warp Speed.4 This was a very, very difficult task. During the trial, critical information would flash by in mere seconds which necessitated that I sit through absolutely everything.
Readers should also know that Grace was not the first child the Scharas lost. They had a son, Travis, who died by suicide in 2018 at the age of 30. Grace’s ‘big brother,’ Travis was a sporty man with a Bachelor’s Degree in Exercise Science who also loved music. Travis was an uncle and ‘friend to many who will miss him dearly.’ (Archive).
After a family of three children, two girls and a boy, the Scharas now have only one child remaining: a daughter named Jessica.
On the stand, Mrs. Schara talked about how when Grace died, there was ‘one fewer plate at the table.’ When Mrs. Schara said this, I received a vivid image of her setting the table for her children when they were young, progressively laying out fewer plates of food as the years passed, the table growing quieter and less joyful as the children disappeared. From three plates in front of a full table of laughing children, to two plates, and then finally: to one plate in front of the last little girl.
Two empty chairs in front of a table that used to be full of laughter.
The tireless activism of the Scharas, both in raising awareness of suicide of one child, and then medical death of another, cannot be overstated. Even through their own pain, these people are providing information so we may save our own families.
Listening to Mr and Mrs Schara testify about Grace, what struck me is how, even in her death, they both lit up with pride at the mention of her name. There was a lot of laughter when they described her stand-up comedy routine, pride when they mentioned her music and dance, and love when they described her closeness with God.
Grace was a young woman who walked with God in a way that most of us cannot even begin to fathom – of this I am certain. Grace, in her wisdom, even described Mr and Mrs Schara as her “earthly mom and dad.” Grace had an implicit understanding that her true home was not on this earth, but in heaven with Jesus Christ.
In October 2021, Grace Schara walked into a hospital under her own steam, was transferred to hospital via ambulance, and never felt the sunshine on her face again. Listening to the testimonies over the course of the trial made me viscerally experience the sheer terror of entering a hospital with the expectation of receiving care and never leaving.
Transcripts were selected based on interest to readers within the remit of ExcessDeathsAU and facilitate deeper understanding of what transpired during the trial.

3. Transcripts: Informed consent in an intensive care unit.
Key words in bold: roles of doctors and nurses, medication, Remdesivir, DNI/DNR, POA, implied consent, iatrogenic injury, expert bioethicist, communication.
Disclaimer: Transcripts manually transcribed by EDAU from Children’s Health Defense links. Mistakes unintentional. Excerpts only. As above, for a full understanding of what occurred during the trial, it is essential to listen to the entire proceedings.
People referenced in below transcripts (does not include everyone involved in trial. See case details here).
Nurse Hollee McInnis, RN. (Defendant) – nurse on duty the day Grace died.
Dr Gavin Shokar, MD (Archive) (Defendant) – physician in charge on the day Grace died.
Alison Barkholtz, RN (Defendant) – lead RN in ICU. Cared for Grace in hospital.
Dr. Gilbert Berdine, MD (Archive) – Expert witness for the plaintiff (Schara family). Believes Grace’s cause of death was not covid but metabolic acidosis caused by ‘overdose’ in the ICU. Berdine believes Grace could have been saved and the Schara family screaming over FaceTime to the nurses to ‘save her’ was an effective verbal removal of the DNR placed on her chart. Did not care for Grace in hospital.
Susan Eichinger, RN – Expert witness for the plaintiff (Schara family). Testified as to many breaches in standard of care by Ascension Hospital. Worked on a covid ward in Florida during Emergency powers. Did not care for Grace in hospital.
Dr David Fisk, MD.,5 infectious disease expert for the defence (Ascension Health et al.). Did not care for Grace in hospital.
Dr Brian Garibaldi, MD (Archive) – pulmonology and critical care expert for the defence. Did not care for Grace in hospital.
Dr Mary Beach, MD (Archive) – Bioethicist and expert for the defence. Berman Institute of Bioethics. Johns Hopkins University. Did not care for Grace in hospital.
Atty Jason Franckowiak: (Archive) - Attorney for the defence.
Atty Randall Guse: (Archive) - Attorney for the defence.
Atty Voiland: Attorney for the plaintiffs.
Atty John Pfleiderer: (Archive) - Attorney for the plaintiffs.
#
Day 3 of trial - Nurse Hollee McInnis, RN.
Time stamp: 1h 16m.
Plaintiff lawyer:6 Did you make an effort to obtain consent for the injection of that medication? [Ed. – Lorazepam].
McInnis: Nurses don’t obtain consent. Obtaining consent is a physician role. Nurses implement orders.7
5h 23m - Dr Gavin Shokar
Atty Franckowiak: Doctor, it’s fair to state that nurses do not conduct informed consent discussions with patients with regards to things like medications, true?
Dr Gavin Shokar: No that’s inappropriate it’s a physician-to-patient communication.
Atty Franckowiak: Ok you were also asked a question there about some of the things that-
Dr Gavin Shokar: Sorry- sorry- can I take that back? Nurse practitioners who are trained to do this can also do it. There’s a lot of good palliative care nurse practitioners. We call them advanced practice nurses that- they can do that as well. So it’s not ‘physician only’ you’re in that ‘practitioner physician’ relationship.
7h 17m – Dr Gilbert Berdine.
Atty Pfleiderer: Doctor. Before the break we were talking about informed consent and I think you listed some items. Just to refresh the jurors would you please hit the points quickly – bullet points.
Berdine: Number one: the goals or purpose of the procedure or therapy must be explained. Number two: the risks of the procedure or therapy must be explained. Three: alternatives to achieve the same goals other than the proposed therapy must be explained. And four: all of those three elements must be documented in the medical record.
Atty Pfleiderer: Who has the obligation to provide that information?
Berdine: The healthcare providers.
Atty Pfleiderer: The physician?
Bernine: Physician, nurse, depending on who’s doing what.
[…]8
Atty Pfleiderer: Thank you, your honour. My point there on informed consent, doctor. Is it the patient’s or the patient’s advocate’s responsibility to go out and seek this information?
Berdine: That’s a com- [Ed. - unintelligible] different people desire different levels of information. And we don’t provide the same level of information to everybody. But in a situation where the pa- [Ed. - unintelligible] states that they want to be informed about every therapy being given to the patient, then you have an obligation to provide that.
#
Day 4 of trial - Dr Berdine
Time stamp: 10m
Atty Pfleiderer: Ok doctor I did want to hit before we get into the case you said something yesterday. We were talking about informed consent and what that meant. You said something about a physician could need to get informed consent or a nurse could get informed consent I think you said ‘depending on what’s going on.’
Prof. Berdine: Yes
Atty Pfleiderer: Are all types of nurses responsible for getting informed consent?
Prof. Berdine: No
Atty Pfleiderer: Ok. What types of nurses are responsible for that?
Prof. Berdine: So the two types that come to my mind would be nurse practitioners and the other situation would be nurse anaesthetists.
#
Day 5 of trial - Nurse Suzi Eichinger
Time stamp: 2h 42m
Atty Franckowiak: Can we agree that nurses in Wisconsin do not have any duty to obtain the informed consent of a patient or a POA for either the administration of medications or the entry of a DNR order, true?
Eichinger, RN: Yes.
#
Day 7 of trial - Dr David Fisk, MD.
Time stamp: 4h 52m
Atty Franckowiak: Would it be practical in an ICU care setting to require for example a physician to contact a patient’s POA to discuss each and every medication, addition, dose, modification, or administration of every common medication before making changes?
Dr David Fisk, MD: No.
Atty Franckowiak: And in fact, is that required as part of the standard of care in an ICU setting in October of 2021 for a physician to have to contact a patient’s POA to discuss each and every medication addition, dose, modification or administration of common medications?
Dr David Fisk, MD: That was not the standard of care in October 2021 nor has it been at any other point in my career.
Atty Franckowiak: Why is that?
Dr David Fisk, MD: It’s something that’s not even feasible first of all. Medication dosages for a range of medications such as blood pressure support medications, medications to help adjust heart rhythms, and medications that are needed in crisis or emergent situations, medications that have to be used if somebody needs to be intubated in order to have a chance to survive, they can’t endure the intubation unless they’re given medications before then.
And so that is an emergent situation at times where it has to be done immediately, or you won’t have a chance to intubate the patient because they will have passed. Really complex patients in the ICU that have often multiple different illnesses or diseases are – they may have hundreds and hundreds of medication dose adjustments in the course of a day from the numerous medicines that are used concurrently to take care of such ill and unstable patients.
Atty Franckowiak: And the use of typically used medications to keep a patient comfortable for example like Precedex and Lorazepam would fall in that category of medications that would not require for example permission from a POA for a dose changes or administration
Dr David Fisk, MD: Yeah I don’t personally prescribe Precedex I do prescribe at times Lorazepam for patients, but certainly those medications are really provided under what I think of as for the general consent for hospital services and care, and that not each time something like that is ordered or administered or dose changed needs consent from a POA requested or obtained.
7h 33m
Plaintiff Atty: If at one point on October eighth, the father was told that Grace wasn’t a candidate for Remdesivir, convalescent plasma, for whatever reason he was told that…later on, if somebody asked to put Grace on Remdesivir or convalescent plasma, he could have had in his head ‘I was already told she’s not a candidate for this – no.’ Is that possible?
Dr David Fisk, MD: Yes. That’s possible, that he could have had that in his head.
Plaintiff Atty: Would that be an informed consent issue?
Dr David Fisk, MD: Um…specifically…um…informed consent in this case is really…for Remdesivir is included with the general consent for hospital services. So prescription of Remdesivir is not something that requires signature of an additional informed consent document. Convalescent plasma, though, is a little different. Convalescent plasma did require a fully-signed informed consent document because it was considered in a more experimental phase although it – even though – it was considered more experimental it was widely used and remains used today.
So the answer to your question is ‘it depends upon which aspect of these therapies that we’re discussing.’ So Remdesivir it’s already covered. Additional convalescent plasma would require additional level of consent and I remember seeing that later on. Convalescent plasma was also recommended for Miss Schara and there was a statement saying that the - although consent discussions were had - the consent document was never signed by Mr Schara.
7h 57m
Atty Franckowiak: The placement of a DNR order in the EMR [Ed. – electronic medical records] was sufficient to comply with the standard of care in October of 2021, true?
Dr David Fisk: Yes absolutely.
Atty Franckowiak: Ok. It [Ed. – DNR order] did not require for instance any particular written document or signature in order to comply with the standard of care for entry in the EMR was sufficient, true?
Dr David Fisk: If the entry was there and is documented by the physician that a consent discussion was had and recorded, yes.
Atty Franckowiak: And in this particular case you saw in the records for example of Dr Shokar that he did indeed have a consent discussion in this particular instance with Mr Schara.
Dr David Fisk: For a DNR you order mean?
Atty Franckowiak: Yes
Dr David Fisk: Yes
Atty Franckowiak: Ok. And that was sufficient to comply with the standard of care for Dr Shokar, true?
Dr David Fisk: Yes
8h 26m
Atty Voiland: Did the standard of care change for the DNR order during covid?
Dr David Fisk: The DNR order?
Atty Voiland: Yes
Dr David Fisk: No it did not change.
#
Day 8 of the trial - Dr Brian Garibaldi, MD
Time stamp: 50m
Atty Guse: Dr Garibaldi does the standard of care require an ICU physician to obtain informed consent before ordering Precedex?
Dr Brian Garibaldi, MD: No
Atty Guse: Why not?
Dr Brian Garibaldi, MD: So informed consent in the term that I think you’re implying is, you know, when we get consent for a specific procedure. So for example if you’re having surgery, or if you’re having a central line placed or if you’re having some sort of invasive procedure. Giving Precedex for sedation in intensive care unit is routine care just like giving an antibiotic would be or giving other medications, so we do not obtain informed consent for the use of Precedex.
Atty Guse: Is the concept of routine care or routine medications encompassed in what might be called ‘general consent?’
Dr Brian Garibaldi, MD: Yeah, there’s something called ‘implied consent’ when you come in to the hospital. So for example if you broke your arm, and you drive yourself to the emergency department, it’s implied that you want to have treatment, and so you don’t have to get informed consent to get your chest x-ray, or to have your cast put on, but if you need surgery, if they need to take you to the operating room and they need to open up your arm and fix the bone, that is an invasive procedure that comes with significant risk, and so that is a procedure that would require informed consent. But placing an IV, doing a chest x-ray, giving routine medicines like antibiotics or even sedatives for agitation in the ICU, that does not require informed consent.
1h 3m
Atty Guse: I know you said in general that consent is not needed for Precedex. As Dr Shokar did not order the medication Precedex, did he have any obligations under the standard of care to have any type of informed consent discussion with the Schara family at any point while he was managing Grace’s care?
Dr Brian Garibaldi, MD: No, there was no requirement for an informed consent discussion.
Atty Guse: Doctor Berdine has testified about two instances early on in Grace’s hospitalisation after Precedex was started where he claims Grace was ‘overdosed.’ Are you aware of those two instances?
Dr Brian Garibaldi, MD: Yes I am.
Atty Guse: Do you agree with doctor Berdine that Grace was ‘overdosed’?
Dr Brian Garibaldi, MD: No. She was not overdosed. She was receiving medications within standard titration parameters…and she…on the first instance on October seventh she experienced a side effect. She had low blood pressure and low heart rate which are known side effects but it’s not an overdose because she was receiving appropriate dosing of the medication at the time and appropriate monitoring.
2h 32m
Atty Guse: Do you have an understanding as to what the standard of care requires of a doctor having a DNR discussion with a patient or a patient’s advocate when that individual is an inpatient in the ICU?
Dr Brian Garibaldi, MD: Yes I do.
Atty Guse: [unintelligible] …doctor does the standard of care require a witness?
Dr Brian Garibaldi, MD: No it does not.
Atty Guse: [unintelligible] …require a document signed by the patient or a patient’s advocate in the patient’s chart?
Dr Brian Garibaldi, MD: No it does not.
Atty Guse: Is the fact that there is an order indicated in the EMR entered by the physician…is that sufficient to document the DNR?
Dr Brian Garibaldi, MD: That plus a documentation of the discussion. Yes.
3h 11m
Atty for plaintiff: We’ve heard testimony in this case doctor that the family members weren’t even told about the drugs they (sic) were receiving so the question that I’m posing to you is in example of morphine, is the standard of care in your opinion even require physicians to tell a patient that they’re going to get morphine?
Dr Brian Garibaldi, MD: And there are multiple points in the chart where there is documentation of describing the reason for both Lorazepam and Precedex.
Atty for plaintiff: Did someone come into the room every morning with a copy of the chart from the day before?
Dr Brian Garibaldi, MD: I don’t believe so, no…I’m not sure what you’re getting at.
Atty for plaintiff: What I’m getting at…that doesn’t mean the family knows it’s happening, right?
Dr Brian Garibaldi, MD: There is indication that there were discussions with the family about the reason to give Lorazepam and the reasons to give Precedex. Those are documented in the chart earlier on in the hospitalisation, and we don’t make distinctions between if it’s ok to give a sedative in one situation and we don’t get permission for each individual sedative.
Alison Barkholtz, RN – defendant
Time stamp: 7h 30m
Plaintiff Atty: You know there’s a fancy word called iatrogenic injury. Do you know what that word means?
Alison Barkholtz, RN: No I don’t.
#
Day 9 of the trial - Dr Mary Beach, MD – Bioethicist
[Ed. - Beach affirms the testimonies of the experts for the defence (above). I strongly recommend those interested in informed consent listen to the entire testimony].
39m
Atty Guse: Based on your review [Ed. – of Dr. Shokar’s notes] do you believe that the DNR order in this case was entered based on the consent of the Shara family?
Beach: Yes.
1h 16m
Juror question (read by judge)
Judge: Mr Schara had asked to be made aware of what medications Grace was receiving. In your opinion, was not telling him – or not telling other powers-of-attorneys – about these drugs in line with the ethics you’ve laid out? Not talking about informed consent, just about telling the patient or the power-of-attorney.
Dr Beach: Oh. Yeah. I think that if someone has asked to know what medications they’re getting, then I think ethically you want to tell them what medications they’re getting.
1h 18m
Atty Franckowiak: Yeah I have just one question. We can agree that nurses do not have a responsibility to obtain informed consent or discuss medications with patients, true?
Dr Beach: Nurses don’t have a responsibility to do informed consent, yes.
#
Day 10 of trial - Dr Gavin Shokar (Defendant).
Time stamp: 7h 56m.
Shokar: …The one thing that came out of the conversation [Ed. – with Scott Schara] that was definitive was that he did not – as a family – they had discussed it from the night before – they got back to me and said – was that they do not want her to be intubated. We had previously talked about futility of CPR in that situation. I reconvened we talked a bit more about it, for, and we went through all the aspects of what CPR, the prognosis – ‘cos – I told them basically, you know, when you’re in a hospital, and you’re a normal patient (or as normal as you can be) your chances of resuscitation with CPR are 23 percent. This is not guarantee. This is someone with no co-morbidities. And this is the conversation I had with him: I said ‘CPR is not a guarantee.’
You can get resuscitated on average twenty-three percent only, and that’s if you have everything going for you. If you have co-morbidities, issues, damage, your chance of resuscitation goes down dramatically, ok? And so if you have an irreversible cause now which is hypoxia or lung damage and you are not fixing that, your chance of resuscitation are almost nil, and even if you somehow get the heart to restart, if will stop again, and you end up in this vicious cycle where you are just jamming on someone’s chest, breaking their ribs, causing trauma, until they die. And so that is the conversation I had with Scott about ‘this will be futile to do, it actually does not look good, it’s gonna cause a lot of more trauma.’ So that was kind of the context of that conversation, and so the end result of that conversation was ‘right we shouldn’t do it if we have a respiratory arrest or respiratory distress.’
Atty Guse: Do you firmly believe, and you’re 100% certain that the DNR order you entered on October 13, 2021 was consented to by the family?
Shokar: I one-hundred percent believe it was consented to, given how extensive the conversations and the detail that went into those conversations beyond that of other DNR/DNI conversations that I’ve had.
#
Day 11 of trial - continuing with Dr. Shokar
Time stamp: 1h 17m
Jury questions (read by judge).
Judge: Do you think the family understood that without intubation, Grace did not have a chance to survive?
Shokar: I do think they knew, but remember, these conversations are extremely difficult. I mean…they also knew that her chance of survival was very low, and, in context where if she were to survive, there was going to be likely fibrosis and damage to the lungs and – what is that going to look like for Grace’s life? This is why we put this conversation to the family members who know her best and say what she would want because that – they’re liaisons to what she would want and so when we have these conversations essentially, there’s no good option in this situation.
These are both…it’s just not…it wasn’t a good situation. So when I have a conversation with Scott about this and his family, it’s to understand that there’s no hundred-percent fix here. There’s a bad option and that option has its risks and its consequences, and so please weigh the considerations. So I felt we had a good discussion and that’s why again there’s no wrong decision in these. I don’t want people to think that there was a wrong decision. These are very tough conversations between provider and patient.
Judge (following up jury question in his own words): I think you answered that ‘you believe they understood that without intubation Grace did not have a chance to survive’ is that accurate?
Shokar: I believe so, but I also believe they felt that she would survive with BiPap and get better [Ed. – BiPap is non-invasive ventilation. At that point Grace was on max. BiPap settings].
Day 11 - Scott Schara
Time stamp: 2h 2m
Atty Voiland: Did anyone from St Elizabeth’s Hospital ever discuss Precedex with you?
Scott Schara: No
Atty Voiland: Did anyone from St Elizabeth’s Hospital ever discuss Lorazepam with you?
Scott Schara: No
Atty Voiland: Is there anywhere in the medical record, that you reviewed, at least ten times, any documentation in the medical record, that anyone from St Elizabeth’s Hospital ever discussed Precedex with you?
Scott Schara: No
Atty Voiland: Is there any documentation in the medical record that anyone from St Elizabeth’s Hospital ever discussed Lorazepam with you?
Scott Schara: No
Atty Voiland: You say that knowing the defence is going to cross-examine you. There’s a document - they’re going to show it to you.
Scott Schara: I presume so.
Atty Voiland: Mr Schara, were you ever actually asked to put Grace on a ventilator?
Scott Schara: Never.
Atty Voiland: From October sixth to October thirteenth?
Scott Schara: Well, let me explain one incident, because when Dr Marada [Ed. – Ramana Marada, listed as a defendant] came in the morning of the eighth, he said ‘you’re going to – you’re going to need to put your daughter on a ventilator in the next two hours’ so that would have been the only time that somebody said that a ventilator was necessary. And that’s when I said at that time ‘what is that recommendation based on’ and he told me that they had done a blood gas the night before, and the time of the blood gas was during the overdose event on the seventh. And so I asked for a blood gas to be redone because that was his source of the recommendation, and he did order a new blood gas, and so a ventilator then was never an issue again.
Atty Voiland: And when we say ‘never an issue again’ did anyone ever again tell you ‘here and now, Mr Scott Schara, you need to place your daughter on a ventilator.
Scott Schara: No
Atty Voiland: Or not even in the way that Doctor Marada had ‘you’ve got two hours to put your daughter on a ventilator.’
Scott Schara: That’s correct.
[…]
Atty Voiland: Dr Shokar did not ever say that to you.
Scott Schara: That’s correct.
Atty Voiland: Now you’ve been asked ‘if someone asked you the only way to save Grace’s life is with intubation, would it have changed your mind?’ Do you remember that?
Scott Schara: I do.
Atty Voiland: What’s your answer to that question?
Scott Schara: The answer to the question is of course I would have changed my mind.
[…]
Atty Voiland: No one ever asked you that did they?
Scott Schara: They did not.
[…]
Atty Voiland: Dr Shokar testified that he told you ‘Grace could crash at any time’ during an October twelfth call, do you remember Dr Shokar testifying to that?
Scott Schara: I do.
Atty Voiland: Did that conversation ever happen?
Scott Schara: No.
Atty Voiland: How do you know that?
Scott Schara: Because that was not the purpose of the October twelfth call. The purpose of the October twelfth call was to introduce himself as the new doctor in charge of Grace’s care, and after that we went through the past. He wanted to hear my version of things that have happened. I talked to him about the faulty equipment situations, and then he went into an elaborate discussion of a ventilator and at that time, what I did, he testified that there were a number of people in the room that I identified, well that isn’t what happened.
When he started getting into the ventilator discussion, I first called – we tried to get a three-way call with a doctor friend of ours because I don’t know anything about a ventilator, so I wanted to have somebody who we trusted hear part of that conversation. She was not available so then we called our pastor, and the reason we called him is because he’s EMT-trained, so I wanted to have somebody on the line who I trusted that would be able to interpret what he’s talking about with a ventilator. And then that conversation closed with that we would take what he said and think about it overnight and he would call the next day.
Atty Voiland: So in this conversation with Dr Shokar, did he ever tell you that if you wouldn’t give him a preauthorisation for a ventilator, that that would mean that he was going to label Grace ‘do not intubate.’
Scott Schara: No
Atty Voiland: And there’s a difference to you, is there not, between a ‘pre-authorisation’ vs actual intubation.
Scott Schara: Definitely.
Atty Voiland: Did Doctor Shokar ever tell you that once he then labelled her ‘do not intubate,’ that also meant to him, he would then place a ‘do not resuscitate’ order in her chart?
Scott Schara: That was never stated, in fact when I was first on the stand here last week I explained very simply if that question would have been posed that way or that statement that way, ‘just so you know, if you don’t want to give us a pre-authorisation for a ventilator, that means DNI to us, and once we label somebody DNI, that means DNR, a DNR order will go on her chart,’ well all kinds of red flags would have went up at that point.
2h 38m - Cross-examination of Scott Schara.
Atty Franckowiak: [Ed. – referring to a letter Scott Schara wrote after Grace’s death]. Mr Schara do you recall writing in that letter “ventilator push from Doctor Marada was the first of five different times the doctors attempted to steer us this way.” Do you remember writing that?
Scott Schara: I do.
3h 6m
Jury asks questions (via judge).
Judge: Did you, or anyone else, give Grace ‘invermitten’ (sic) [Ed. – ivermectin]. If not, why. If yes, why did she get worse?
Scott Schara: Yeah that’s a great question. Yes, we did give Grace ivermectin. We had gotten a prescription for ivermectin I think plus or minus October first before we tested her because we saw she had symptoms, and then we gave her ivermectin. So then the question is ‘why didn’t she get better?’ The answer to that question is a little bit more detailed. First of all I don’t know why she didn’t get better. It’s not a silver bullet, so no med can ever fix something instantly.
Why didn’t she get better? I don’t know that she was getting worse. We were fixated on Grace’s oxygen saturation, and you might remember we had bought a pulse oximeter, and we were measuring Grace’s oxygen saturation, and on the morning of October sixth it had dropped to about eighty-eight percent. And, the protocol that we were following at the time said that that’s an emergency – admit yourself to the hospital. And so this was by the Front Line Covid Critical Care doctors – we were following that protocol and it said ‘if the oxygen saturation got to eighty-eight percent admit yourself to the hospital.’
At the time we went to the hospital, I would have looked at Grace’s symptoms as allergies. She had a cold, she had allergies, there was no emergency but we perceived the emergency that was based on her oxygen saturation.
[End transcript excerpts by EDAU]
4. Bonus mini-transcript: Nurse Alison Barkholtz makes a slur in court and nobody objects.
Time stamp: 7h 49m
Atty Franckowiak: I believe there may have been some – maybe it’s just terminology – but there may have been some mischaracterisations there. To your knowledge, was anyone exempt from visitor policies?
Nurse Alison Barkholtz: In regards to…what are you referring to? Like they get to be an asshole?9
5. Final thoughts
Listening to the entirety of this trial, it has never been starker that humanity’s perception of reality in 2025 has not just been divided but shattered.
There are those in society who accept the mainstream covid narrative – that medical staff were heroes saving lives during a deadly pandemic. Then there are those who accept that the protocols themselves were dangerous and hastened death. Many people fall somewhere in between these two groups.
Regular readers of ExcessDeathsAU know that I have written multiple articles about the new hospital and care home protocols deployed during global military program Operation Warp Speed. For a bullet point list, please see “25 COVID Protocol Commonalities” at the covid-19 Humanity Betrayal Project.10
However, even before Operation Warp Speed, mainstream media outlets (archive) were sounding the alarm on how (e.g.) hundreds of thousands of Americans may be potentially dying at the hands of the medical profession in a ‘normal’ year, claiming that ‘medical error’ may be the third leading cause of death in the US. These same mainstream media outlets proclaimed in 2018 “that physicians, funeral directors, coroners and medical examiners rarely note on death certificates the human errors and system failures (were) involved.”
Medical journals that warned about iatrogenic deaths before ‘covid’ quickly pivoted to a whole-of-society capture in 2020 where questioning ‘the science’ meant you were a murderer and had to be censored, shunned, and evicted from society.
In the transcripts presented, we saw that one of senior medical staff from Ascension Health who took the stand (Alison Barkholtz, lead RN in St Elizabeth intensive care unit) did not even know the definition of ‘iatrogenic.’ These are the people who are caring for us and our families at our most vulnerable.
In terms of informed consent, this trial was critical for exposing the reality of what happens in the ICU both during and outside of Emergency powers. For those who work in this space, I strongly recommend listening to the entire trial and obtaining official court transcrips as well as the legal and policy documents referenced throughout.
Every expert medical witness, including those from the plaintiffs, testified that in an ICU setting in the US, “nurses do not obtain informed consent - nurses implement physician orders.”11 We also learned about ‘implied/general consent’ in a hospital and how patients are given medications/doses without being told.
We learned from Dr Fisk, expert witness for the defence, that:
Remdesivir is included with the general consent for hospital services. So prescription of Remdesivir is not something that requires signature of an additional informed consent document.
This is how ‘informed consent’ works in the real world.
In terms of ‘covid times,’ multiple realities have occurred because of the mountain of lies and contradictions from governments about what happened, particularly in early 2020. Governments created a false reality that was repeatedly contradicted to the point of absurdity. In my opinion, the incredible culture of fear, purveyed by both governments and the ‘alt. media’ drove people to panic that killed millions and tortured billions around the world.
In 2025, few agree on how people got sick, how they died and, increasingly, even on the very nature of matter and reality. Few of us are on the same page even if we are in the same broad ‘sphere.’ There has been no healing because people are trying to piece together what happened blindfolded with one arm tied behind their backs. We are swimming in the mire of hypernormalisation.12
However, even if governments were to tell the ‘truth,’ at this point increasingly few would believe them. Many people will remain suspicious about government and institutional narratives and the people around them – their own communities and even families - for the rest of their lives.
In the specific case of Miss Grace Schara, these multiple realities clashed in a courtroom in Wisconsin, creating doubt and contradiction not just broadly from the plaintiff or the defence, but often from the same witness. The upshot of this trial was that, in the eyes of jury according to the parameters of the case, this doubt became legally insurmountable.
Again, I would encourage everyone to carefully listen to the entire trial so they can form their own opinion of what occurred in the courtroom. If one does not have the time to listen to the entire trial, I would encourage readers to listen to the closing arguments, which summarise the trial.
Closing arguments occurred on day 13 and begin with the judge providing instructions to the jury. It is important to listen to this to understand the parameters of the case from the perspective of the jury particularly regarding standard of care.13
On day four of the trial (7h 55m 40s) Judge McGinnis said the following to both legal teams after the jury was dismissed for the day:
Judge: How often, Mr Guse, do you have jurors ask questions?
Mr Guse: Not very often.
Judge: Right. And look how good it’s been. I think each witness has looked at the jurors and said ‘that’s a really good question. It’s a good question.’ And they’re questions that they obviously want, they’re going to help them get the results.
Mr Schara first answered the jury’s questions on Day 2 (7h 30m-7h 48m) and described the jury’s questions as ‘fantastic’ (three times), ‘good’ (twice), and ‘insightful’.14
After the verdict on day 13 (time stamp 8h 52m), the judge was also very clear that there was a high police presence in the courtroom/courthouse and was attentive to jury concerns about their safety (real, potential, and/or perceived - during and after the trial) given the high-profile nature of the case.
Whatever one’s sphere of reality and experience, mass death and trauma has occurred, and people are angry, depressed, confused, and frightened. A global military campaign called Operation Warp Speed murdered millions and poisoned billions via multiple deployed countermeasures across numerous theatres of war.
One of those theatres of war was the hospital setting that began in 2020. In the US, hospital staff were given blanket indemnity for injuries and deaths during Emergency powers starting March 1, 2020 under the Trump administration, setting up the hospital and care home protocols not just in the US but around the world:
Cognitive warfare divided us and locked us down and still has us at each other’s throats, and in many cases, questioning the reality we have always taken for granted.
Now we witness-survivors are left holding the bag in the ‘new normal’ that was promised, blinking in the glittering light of a pale dawn none of us ever wanted.
With fewer plates and empty chairs at everyone’s tables.
After the verdict, the judge had this special message in the courtroom for the Schara family:
I never met Grace, but I’m glad I got to be a part of her for these past three weeks, in a sort of unfortunate way. I know that the world was a better place with her in it, and our community was. Good luck to everybody.
I feel exactly the same way, and extend my love to the Schara family and all my readers who lost someone in the hospitals and care homes during Emergency powers.
God Bless you readers, and good luck to everybody.
Until next time.
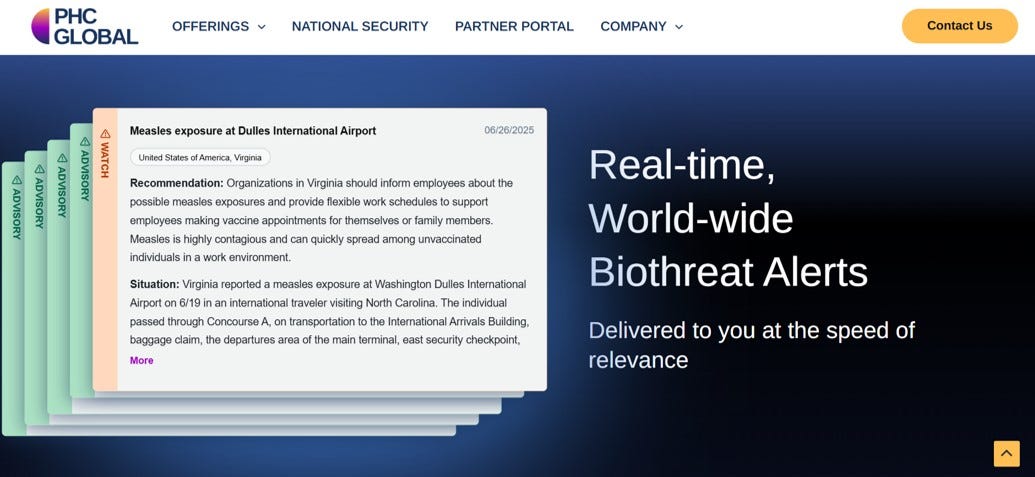
Postscript: Building the future of Biodefence at the speed of relevance with Dr David Fisk, MD., expert witness for the Defence in the Grace Schara case.
Dr David Fisk (MD) is an infectious disease specialist serving as the medical director of infection prevention and control at Cottage Health in California. Fisk leads the infection control team at Cottage, working with physicians and hospital leaders on the COVID Incident Command Center to “ensure the highest level of preparation and care for patients”. (Archive).
Dr Fisk is also Chief Medical Officer at PHC Global: (Archive)
PHC Global is at the forefront of biosecurity intelligence, providing early warning in the face of emerging biological threats to protect humankind and capital. PHC Global is the first to develop a Software-as-a-Service (SaaS)-enabled solution that combines proprietary data with tactical and strategic intelligence to empower enterprises to protect employee safety, business continuity, and economic security. Founded by visionary Dr. Charity Dean, PHC Global harnesses the power of world-class experts and cutting edge machine intelligence to deliver actionable intelligence with unmatched speed, scale, and accuracy.
PHC is “building the future of biodefence…biothreat intelligence to deter and detect natural, accidental, deliberate and novel biological agents…to protect(s) the warfighter and mission-critical assets at home and abroad.” One of the company’s services is notification of “real-time world-wide biothreat alerts delivered at the speed of relevance.”
As an infectious disease specialist, Dr. Fisk testified for the defence in the Grace Schara case about many subjects, mainly related to his experience treating covid patients in an ICU setting. He also opined on vaccines and medications such as Remdesivir. As per the article above, readers are encouraged to listen to the entire trial to form their own opinion. However, below are some brief transcripts of Dr. Fisk’s testimony.
Dr David Fisk, MD develops pandemic hospital visitation policies.
Time stamp: 5h 16m.
Atty Franckowiak: As an infectious disease specialist working in hospitals in late 2021 would you be familiar with hospital visitation policies related to covid 19 as they existed at that time?
Fisk: Yes. I was not only familiar with them I helped develop those protocols and policies for my institution as part of the incident command team for the health system.
Atty Franckowiak: According to your experience, were hospital policies that restricted visitation widespread during the covid pandemic?
Fisk: Yes, actually they were very widespread and in many places mandated by health departments.
Dr David Fisk, MD opines on emergency use authorisation.
8h 30m
Atty Voiland: Do all emergency use authorisation therapies require informed consent because they are experimental?
Fisk: Many of them are…it depends by what you mean by ‘informed consent.’ Do they require separately signed consent documents? No. When they’re under emergency use authorisation. So for example, we regularly prescribed Remdesivir, or Regeneron, or other things when they were under the emergency use authorisation phase before they had full FDA approval without additional consent documents being signed. We did have discussions with the patients or their representatives, and in those discussions went over the risks and benefits and the fact that the drug did not necessarily have full FDA approval.
Dr David Fisk, MD opines on covid vaccines.
Time stamp: 2h 37m
Atty Franckowiak: Thank you doctor. According to your experience with covid as an infectious disease expert, did Grace Schara in October of 2021 have any specific risk factors that you believe placed her at an increased risk of experiencing severe covid or death from covid?
[Fisk speaks to obesity]
Fisk: …she also had not been vaccinated for covid, and at that time [Ed. – October 2021] the covid vaccines offered roughly a 90% reduction in the chance of dying from covid, so she had not been vaccinated. That led her risk to be higher than someone who would have been vaccinated at that time.
Atty Franckowiak: And were those…was that validated by studies at the time of the vaccines that were available as of October 2021?
Fisk: Yes, yes that was documented in a range of studies for the different vaccines that were available and high-quality studies that have been…we call ‘randomised clinical trials’ which are the type of study that in the world of interpreting medical literature are (sic) provide the greatest degree of…greatest degree of evidence…for a desired outcome.
#
Please now see an article (with video) in 2020 where Fisk urges caution about the covid vaccine. The article advises US military personnel to “do their own research…if benefits outweigh risks.” Key excerpts:
Title: Infectious Disease expert injects word of caution over COVID-19 trial vaccine, Beth Farnsworth, November 10, 2020. KEYT News Channel 3. (Archive).
The first Emergency Release of the trial vaccine includes up to 10,000 doses for Vandenberg Air Force Base (VAFB) within the next month, on a voluntary basis. However, VAFB military participants are advised to do their own research to determine if the benefits outweigh the risks.
Fisk said while this is exciting news -- a trial vaccine touted as having a 90% efficacy rate -- the “critical missing piece of this puzzle" is about safety.
“Right now, it is so vitally important that any COVID vaccine that comes out be safe because it's going to be used so widely in a wide range of individuals, some of who were previously healthy at the time they received the vaccine,” said Fisk.
“Most vaccine side effects that happen, happen immediately or shortly after the vaccine is administered,” said Fisk. “But certainly there are plans for looking for side effects of any vaccine that's approved, for two years after its initial Emergency Release and approval."
Fisk said the fact that Pfizer's vaccine announcement came from a "company media report" rather than a scientific study makes him and others especially cautious.
#
Dr David Fisk, MD opines on Remdesivir.
Day 7. Time stamp: 8h 43m
Question from juror (via judge who is reading the question).
Judge: Is that drug [Ed. – Remdesivir] used as the infusion drug given to patients who had covid vaccine shots if not, what was?
David Fisk: Infusion meaning intravenous administration. Yes, that drug is provided as an intravenous drug. There are also other medications that are provided and offered intravenously.
Judge (following up in own words): So that would have been given to somebody who would have had a covid vaccine shot?
David Fisk: Yes, whether somebody had a covid vaccine or not doesn’t impact whether they were administered a drug like Remdesivir. It’s really based upon their status of being admitted to a hospital and having covid severe enough to require hospitalisation.
#
Please see EDAU article published May 28, 2024 – Remdesivir situation in Australia even outside Emergency powers.
National Clinical Evidence Taskforce COVID-19: DRUG TREATMENTS FOR AT RISK ADULTS WITH COVID-19 WHO DO NOT REQUIRE OXYGEN v 6.0 27 March 2023.
Vaccination status is key to risk assessment:
low risk is associated with symptomatic treatment / observation
for higher risk (including being unvaccinated) Paxlovid is recommended if within 5 days of symptom onset together with Remdesivir if within 7 days.
July 16, 2025: Unlike the transcripts in subsequent sections, these ‘four points’ were paraphrased and did not adhere to transcript accuracy.
I wrote when the court was in recess and the live feed was blacked out
readers will meet him later
At the beginning of my transcribing I did not have the case details and attorneys are indicated ‘generically.’
This statment was confirmed a second time at 1h 24m
Plaintiff lawyer: And were you required to obtain consent for that medication?
McInnis: Nurses don’t obtain consent. We implement orders.
indicates irrelevant dialogue
Just so you do not think I am making this up, others following the case picked up on this as well:
Exception to this is specialised nurses (eg., nurse practitioners).
Unfortunately some of the audio – particularly from Mr Franckowiak - is extremely poor
For example, jurors questioned the expiry dates of medical policy documents shown in exhibits, wanted to know all the potential side effects of the drugs Grace was on, and everything she was exposed to in the hospital including left-field questions of defence experts like ‘potential allergic reactions to the plastics in the feeding tube’.