Be Careful What You Say
How honesty leads to the trauma of unnecessary psychiatric hospitalization
Picture a soul in turmoil, wrapped in the suffocating embrace of despair. In the sanctuary of a therapist's office, they finally find the courage to voice the unspeakable:
"Sometimes, I think about not being here anymore."
The words hang heavy in the air, a testament to the crushing weight of their pain, loneliness, and emptiness. This confession, born from a place of vulnerability and trust, should be the beginning of a deeper healing journey.
During these intense emotional struggles, it's important to understand that thoughts of escape, including suicide, are a common human response to overwhelming pain. There's a vast chasm between contemplating an end to suffering and actively planning to end one's life.
Context is everything.
The mind, overwhelmed by anguish, may grasp at any perceived exit, including the idea of nonexistence. But voicing these thoughts doesn't signal imminent danger. Rather, it's often a cry for understanding, a desperate reach for connection in the depths of isolation.
Skilled and experienced therapists understand this.
The very act of sharing these dark musings with a trusted professional can be profoundly cathartic. It's in these raw, unfiltered moments that true therapy has the potential to work its magic. A skilled therapist, one who can navigate these turbulent waters without succumbing to panic, becomes a lifeline. They offer not just a listening ear, but a steady hand to guide the patient through the storm, helping them to contextualize their pain and find hope in the midst of despair. This is the essence of healing - not in avoiding the darkness, but in facing it together, unafraid.
Fast forward to mental healthcare in 2024.
As the demand for mental health services skyrockets, we're witnessing a disturbing trend: the proliferation of ill-equipped therapists flooding the market. What was once a skilled profession has, in many cases, devolved into little more than paid listening.
This watered-down version of therapy lacks the nuanced expertise needed to effectively navigate complex clinical issues, leaving those suffering adrift in a sea of platitudes and superficial interventions.
The rise of virtual therapy platforms, while increasing accessibility, has created a cohort of isolated practitioners. Lured by the promise of higher profits without the overhead of a physical office, many therapists now find themselves cut off from the vital support networks of supervisors and mentors. Without this crucial guidance, they're left to navigate treacherous emotional waters alone, often defaulting to a "cover your ass" mentality when confronted with challenging situations.
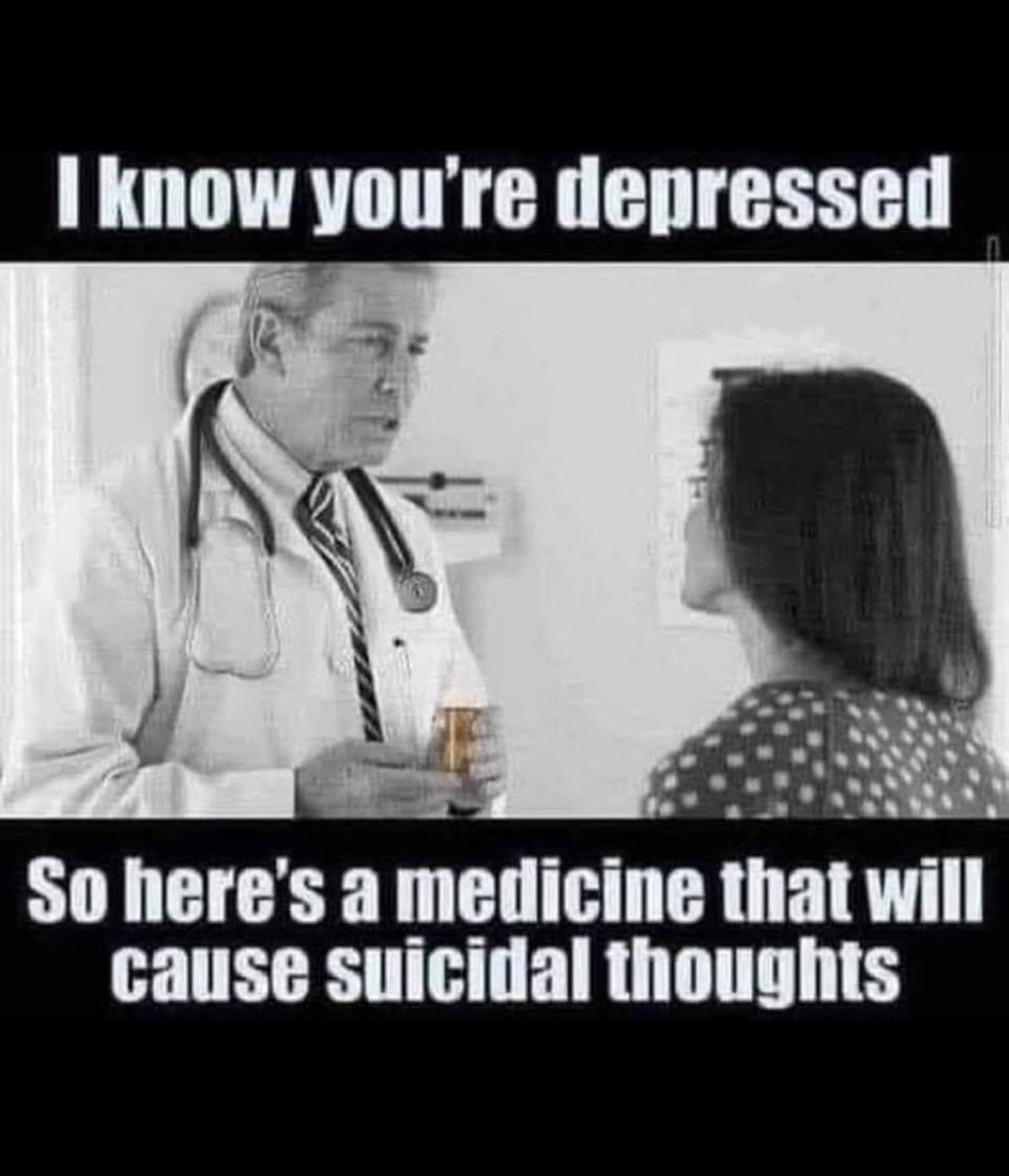
Simultaneously, as large hospital networks muscle into the mental health arena, therapy is increasingly reduced to an appendage of psychiatry. The nuanced art of healing is replaced by a simplistic "take your pills and manage your mental illness" approach. This medicalization of human suffering is fundamentally dehumanizing, reducing complex emotional states to mere chemical imbalances.
The consequences of this shift are stark. Individuals brave enough to voice thoughts of death are no longer met with understanding, but with fear. Their pain is hastily labeled as emerging "mental illness," triggering a rigid psychiatric protocol that leads to overmedicalization and unnecessary hospitalization.
"I want you to go to the emergency room"
The knee-jerk mantra of risk-averse therapists and doctors who've been brainwashed to treat every fleeting suicidal thought like a ticking time bomb.
They herd the emotionally vulnerable into sterile, overpriced hospital rooms, mistaking cold fluorescent lights and paper gowns for actual care. It's a convenient way to abdicate responsibility, slap a band-aid on deep-seated pain, and pad the pockets of our broken healthcare system - all while patting themselves on the back for "saving lives."
A Rise In Psychiatric Hospitalizations
The U.S. mental health care system is at a breaking point, buckling under the weight of an insatiable demand for inpatient care. Recent federal data, as reported by CBS News, reveals a system in crisis: hospitals and clinics are operating at a staggering 144% capacity for inpatient psychiatric beds. This alarming statistic, courtesy of the Substance Abuse and Mental Health Services Administration (SAMHSA), exposes the raw nerve of a long-festering problem - a dire shortage of psychiatric inpatient facilities.
Yet, this begs a crucial question: Is this surge in demand a genuine need, or merely a symptom of a more insidious systemic failure?
The COVID-19 pandemic has cast a long shadow over youth mental health, with alarming consequences. A recent study comparing mental health emergency admissions among young people before and after the outbreak reveals a disturbing trend. In the two years following March 2020, youth psychiatric emergencies surged by an astonishing 116.7% compared to the same period in 2018-2020. Even more concerning, this new wave of patients skewed younger and were less likely to have prior psychiatric histories.
These findings suggest a troubling shift: the pandemic appears to have triggered new, earlier onset psychiatric manifestations in previously unaffected youth. Moreover, these emergencies lead to psychiatric drugs as a matter of course.
Which leads to worsening outcomes.
Primary Care Driving Hospitalizations
The mental health crisis among youth has been sensationalized to a dangerous degree, leading to misguided interventions that may do more harm than good. In pediatric offices across the country the use of quick, invalid screening measures that reduce complex emotional states to simple checkboxes is the primary assessment approach. These cursory assessments, administered by primary care doctors ill-equipped to handle nuanced mental health concerns, are causing undue panic.
A single checked box on these questionable screening measures can set off a chain reaction of fear-mongering, with parents being urgently directed to emergency rooms for what may be nothing more than typical teenage angst or temporary emotional struggles. This knee-jerk approach not only overwhelms emergency services unnecessarily but also risks pathologizing normal developmental experiences.
The media's portrayal of primary care doctors drowning in a youth mental health crisis obscures a more insidious reality: these physicians, despite their best intentions, are conducting mental health evaluations in alarmingly short timeframes without the proper training to contextualize their findings.
The result is a perfect storm of misunderstanding, where the vulnerability and complex emotions inherent to adolescence are stripped of their context and hastily labeled as mental health emergencies. This approach not only fails to address the real needs of struggling youth but also potentially traumatizes families and clogs a healthcare system already stretched to its limits.
Even if these youth are not hospitalized they are going to placed on a drug that will at least double the risk of suicide, if not more. Lexapro is often prescribed despite the 6-fold increase in suicide risk!
The Trauma of Psychiatric Detention
When desperate parents drag a sullen teenager to the ER, or a vulnerable adult finds themselves cornered by an ER social worker, a grim dance begins. The fluorescent-lit stage is set for a performance of "crisis management theater," where real human suffering collides with bureaucratic checklists and liability concerns.
Parents, gripped by fear that their child might take their own life, often feel coerced into consenting to psychiatric hospitalization and medication. This fear becomes a potent weapon wielded by hospital staff, despite the lack of evidence that such interventions actually prevent suicide.
Ironically, within academic circles, it's widely acknowledged that these very interventions may increase the likelihood of suicide. This grim reality makes a perverse kind of sense: patients are prescribed powerful, mood-altering drugs and then discharged back into the very circumstances that initially drove them to contemplate suicide.
The experience of psychiatric detention is frequently described as traumatizing. Patients are stripped of their dignity - quite literally during invasive searches - and their autonomy, as their phones and personal belongings are confiscated. Many report being treated like cattle by burned-out, unprofessional staff.
Young women often feel unsafe, surrounded by men who are also experiencing mental health crises. For women struggling with the aftermath of sexual violence - a common precursor to psychiatric hospitalization - the hospital stay itself can be profoundly re-traumatizing.
This system, designed ostensibly to help, often inflicts further harm. It substitutes genuine care and understanding with a one-size-fits-all approach that prioritizes risk management over true healing. In our rush to "do something," we've created a revolving door of trauma, where those seeking help often emerge more damaged than when they entered.
When parents, armed with knowledge and a desire to protect their children from potentially harmful interventions, attempt to resist the pressure to medicate, they're often met with a dismissive and exasperated "What do you want us to do then?"
It exposes a mental health apparatus that has become reliant on the false promise of quick-fix pharmaceutical solutions, lacking the resources, training, or willingness to explore alternative approaches. This attitude effectively holds families hostage: either accept potentially harmful psychiatric drugs or be left with no support at all.
This false dichotomy - drugs or nothing - is a damning indictment of a system that has lost sight of its purpose. It reveals a profound lack of creativity and compassion in addressing mental health crises. Instead of working collaboratively with families to develop comprehensive, individualized care plans, hospital staff often default to a one-size-fits-all approach that prioritizes expediency over efficacy.
Moreover, this response subtly shifts blame onto the parents, implying that by refusing medication, they're somehow obstructing their child's care. It's a manipulative tactic that exploits parental fear and guilt, further eroding trust between families and mental health providers.
Fear Based Therapy
The mental health industry has a dirty secret: it's terrified of the patients it claims to help. Therapists, those supposed bastions of understanding and support, turn into protocol-driven robots at the mere whisper of suicide. Gone is the empathy, replaced by a checklist of CYA questions designed more to protect their licenses than to save lives.
This is how they are trained.
This fear-based charade masquerading as care has created a toxic environment where honesty is punished. Patients learn quickly: bare your soul at your own risk. Admit to dark thoughts, and watch your therapist's eyes glaze over with panic as they mentally rehearse their mandatory reporting script.
In my years of specializing in treating chronically suicidal clients, I've witnessed firsthand the deep-seated trauma inflicted not just by their original experiences, but by the very system purporting to help them.
A disturbing pattern emerges, particularly among women survivors of sexual violence. Their acute trauma reactions are frequently misunderstood and hastily misdiagnosed as bipolar disorder or other psychiatric illnesses, leading to a cascade of inappropriate treatments and interventions. The psychiatric hospitalizations that often follow are not just ineffective; they're actively traumatizing.
When these survivors finally find their way to my office, the damage is palpable. Trust, the very foundation of effective therapy, has been shattered by their previous encounters with mental health professionals. It can take months of patient, careful work to rebuild that trust, to convince them that it's safe to be open and honest in therapy. This process is painstaking, requiring us to undo layers of iatrogenic harm - harm caused by the very institutions and individuals tasked with healing.
The tragedy here is twofold: not only are these women denied proper care for their actual traumas, but they're also subjected to a secondary trauma at the hands of a mental health system that fails to recognize the complexities of their experiences. This cycle of misdiagnosis, inappropriate treatment, and subsequent re-traumatization doesn't just delay healing - it actively impedes it, sometimes for years. Many never recover.
What Genuine Help Looks Like
True healing begins with the compassionate ear of a skilled, experienced therapist who can create a safe space for emotional expression and validation. This approach recognizes a fundamental truth: everything, including emotional pain and suicidal thinking, is temporary. By understanding struggles in their proper context, therapists can help clients navigate their darkest moments without resorting to extreme measures.
A competent therapist knows that most expressions of suicidal thoughts are not declarations of intent, but rather desperate attempts to communicate profound suffering. This nuance, while seemingly obvious, often eludes less experienced or inadequately trained professionals who are paralyzed by fear and uncertainty. Instead of reacting with panic, skilled therapists help clients explore their pain and envision a life worth living, even in the midst of emotional turmoil and trauma.
When someone is in emotional turmoil and suicidal risk is present, truly skilled therapists know that a gentle, personalized approach can make all the difference. Instead of rushing to hospitalization, these compassionate professionals take the time to really listen and understand. They work hand-in-hand with the person in crisis, crafting a safety plan that feels right and makes sense for their unique situation. It's not about imposing rules, but about finding inner strength and support.
Effective therapy often involves teaching clients how to regulate intense emotions and tolerate distress. This might include techniques drawn from dialectical behavior therapy (DBT) or other evidence-based approaches. For many, additional support such as telephone coaching and family-based therapies can create a plan to weather crisis periods. These interventions recognize that suicidal crises tend to be episodic and often resolve when the underlying problems are addressed.
Primary care doctors should not be administering mental health screening measures or prescribing psychiatric drugs for complex emotional issues. Their well-intentioned but misguided interventions often exacerbate the situation, medicalizing normal human experiences and setting patients on a path of unnecessary and harmful treatments.
Working in “mental health” requires patience, understanding, and a willingness to sit with discomfort – both from the client and the therapist. By moving away from a fear-based, reactionary model of care towards one that embraces complexity and prioritizes genuine human connection, we can create a mental health system that truly serves those in need.
When the storm of the mind rages, feel-good therapy buzzwords and empty reassurances are as useful as a paper umbrella in a hurricane. What's needed isn't another degree or certification, but something far rarer: the guts to stare unflinchingly into the abyss of another's pain without flinching. In the end, perhaps the most radical act in modern mental health care is simply having the backbone to shut up, sit down, and bear witness to suffering without trying to sanitize it.